Connect With Us
Blog
What to Do if You Break a Toe
 A broken toe usually involves something heavy dropping on it or stubbing it on a piece of furniture or another hard surface. The result is bruising and swelling that makes it difficult or impossible to wear shoes due to the pain. Frequently, the patient walks with a limp if they can walk at all. It can take up to 6 weeks for a broken toe to fully heal. Here are a few measures you can implement at home to help with the healing process. First, stay off the foot, and then wrap it to keep the swelling down. Keep ice on the affected toe and elevate it as often as possible. You also may need to take over-the-counter pain medication. Whether your toe is broken or sprained, it is a good idea to consult a podiatrist who can determine the severity of the injury. The foot specialist will take an X-ray and depending on the results, wrap the injured toe to toe next to it (known as buddy taping) as a splint for stabilization. A hard boot may be prescribed to keep the toe safe from further injury. Walking aids, such as crutches, may also be recommended to help keep weight off the toe. In severe cases, surgery may be required.
A broken toe usually involves something heavy dropping on it or stubbing it on a piece of furniture or another hard surface. The result is bruising and swelling that makes it difficult or impossible to wear shoes due to the pain. Frequently, the patient walks with a limp if they can walk at all. It can take up to 6 weeks for a broken toe to fully heal. Here are a few measures you can implement at home to help with the healing process. First, stay off the foot, and then wrap it to keep the swelling down. Keep ice on the affected toe and elevate it as often as possible. You also may need to take over-the-counter pain medication. Whether your toe is broken or sprained, it is a good idea to consult a podiatrist who can determine the severity of the injury. The foot specialist will take an X-ray and depending on the results, wrap the injured toe to toe next to it (known as buddy taping) as a splint for stabilization. A hard boot may be prescribed to keep the toe safe from further injury. Walking aids, such as crutches, may also be recommended to help keep weight off the toe. In severe cases, surgery may be required.
A broken toe can be very painful and lead to complications if not properly fixed. If you have any concerns about your feet, contact one of our podiatrists from Palm Beach Foot & Ankle. Our doctors will treat your foot and ankle needs.
What to Know About a Broken Toe
Although most people try to avoid foot trauma such as banging, stubbing, or dropping heavy objects on their feet, the unfortunate fact is that it is a common occurrence. Given the fact that toes are positioned in front of the feet, they typically sustain the brunt of such trauma. When trauma occurs to a toe, the result can be a painful break (fracture).
Symptoms of a Broken Toe
- Throbbing pain
- Swelling
- Bruising on the skin and toenail
- The inability to move the toe
- Toe appears crooked or disfigured
- Tingling or numbness in the toe
Generally, it is best to stay off of the injured toe with the affected foot elevated.
Severe toe fractures may be treated with a splint, cast, and in some cases, minor surgery. Due to its position and the pressure it endures with daily activity, future complications can occur if the big toe is not properly treated.
If you have any questions please feel free to contact our offices located in Boynton Beach, Palm Beach Gardens, and West Palm Beach, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
What to Know About a Broken Toe
Trauma to the foot, especially the toes, can occur in many ways. Banging them, stubbing them, or dropping something on them are a few different ways this trauma can occur. Given the fact that toes are positioned in front of the feet, they typically sustain the brunt of such trauma. When trauma occurs to a toe, the result can be a painful break or fracture. Another type of trauma that can break a toe is repeated activity that places stress on the toe for prolonged periods of time.
Broken toes can be categorized as either minor or severe fractures. Symptoms of minor toe fractures include throbbing pain, swelling, bruising on the skin and toenail, and the inability to move the toe with ease. Severe toe fractures require medical attention and are indicated when the broken toe appears crooked or disfigured, when there is tingling or numbness in the toe, or when there is an open, bleeding wound present on the toe.
Generally, a minor toe break will heal without long-term complications. However, it is important to discontinue activities that put pressure on the toe. It is best to stay off of the injured toe and immediately get a splint or cast to prevent any more additional movement of the toe bones. You can also immobilize your toe by placing a small cotton ball between the injured toe and the toe beside it. Then, tape the two toes together with medical tape. Swelling can be alleviated by placing an ice pack on the broken toe directly as well as elevating your feet above your head.
Severe toe fractures may be treated with a splint, cast, and in some cases, minor surgery, especially when the big toe has been broken. Due to its position and the pressure the big toe endures with daily activity, future complications can occur if it is not properly treated. Pain associated with minor toe fractures can be managed with over-the-counter pain medications. Prescription pain killers may be necessary for severe toe fractures.
The healing time for a broken toe is approximately four to six weeks. In severe cases where the toe becomes infected or requires surgery, healing time can take up to eight weeks or more. While complications associated with a broken toe are immediately apparent, it is important to note that there are rare cases when additional complications, such as osteoarthritis, can develop over time. You should immediately speak with your podiatrist if you think you have broken your toe due to trauma. They will be able to diagnose the injury and recommend the appropriate treatment options.
What Is Peripheral Neuropathy?
Peripheral neuropathy is nerve damage within the peripheral nervous system, which communicates with the central nervous system (involving the brain and spinal cord). Diabetes often causes peripheral neuropathy, however, it can also occur due to genetics, infections, injuries, hormonal imbalances, or other medical conditions. Peripheral neuropathy may cause numbness, weakness, muscle twitching or cramps, changes in nails, skin and hair, and a pins-and-needles sensation in the legs and feet. It may also be difficult to maintain balance or feel changes in temperature or pain, and you may experience disturbances in your emotions and sleep patterns. If you have any of these symptoms, it is suggested that you contact a podiatrist. They can help diagnose peripheral neuropathy and manage its symptoms with oral medications, orthotic devices, regular checkups and advice on proper foot care.
Neuropathy
Neuropathy can be a potentially serious condition, especially if it is left undiagnosed. If you have any concerns that you may be experiencing nerve loss in your feet, consult with one of our podiatrists from Palm Beach Foot & Ankle. Our doctors will assess your condition and provide you with quality foot and ankle treatment for neuropathy.
What Is Neuropathy?
Neuropathy is a condition that leads to damage to the nerves in the body. Peripheral neuropathy, or neuropathy that affects your peripheral nervous system, usually occurs in the feet. Neuropathy can be triggered by a number of different causes. Such causes include diabetes, infections, cancers, disorders, and toxic substances.
Symptoms of Neuropathy Include:
- Numbness
- Sensation loss
- Prickling and tingling sensations
- Throbbing, freezing, burning pains
- Muscle weakness
Those with diabetes are at serious risk due to being unable to feel an ulcer on their feet. Diabetics usually also suffer from poor blood circulation. This can lead to the wound not healing, infections occurring, and the limb may have to be amputated.
Treatment
To treat neuropathy in the foot, podiatrists will first diagnose the cause of the neuropathy. Figuring out the underlying cause of the neuropathy will allow the podiatrist to prescribe the best treatment, whether it be caused by diabetes, toxic substance exposure, infection, etc. If the nerve has not died, then it’s possible that sensation may be able to return to the foot.
Pain medication may be issued for pain. Electrical nerve stimulation can be used to stimulate nerves. If the neuropathy is caused from pressure on the nerves, then surgery may be necessary.
If you have any questions, please feel free to contact our offices located in Boynton Beach, Palm Beach Gardens, and West Palm Beach, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Ways to Treat Toenail Fungus
 Signs that you may have contracted a fungal toenail infection are rather easy to spot. Typically, you will notice a whitening or yellowing of the nail, and it will appear to be thicker and more brittle. The fungus, known as onychomycosis, is often spread in swimming pools, saunas, gyms, or nail salons – places where you are likely to walk barefoot. Tight socks that hold in moisture may also be a contributing factor. Heat, humidity, and perspiration help spread the infection, which is highly contagious. A few natural remedies that may help reduce the fungus from spreading include applying tea tree, lavender, lemon, or thyme oils to the affected nails. A foot bath with baking soda or white vinegar may help too. However, if the nail condition persists or spreads it is suggested that you consult with a podiatrist for an examination and treatment plan.
Signs that you may have contracted a fungal toenail infection are rather easy to spot. Typically, you will notice a whitening or yellowing of the nail, and it will appear to be thicker and more brittle. The fungus, known as onychomycosis, is often spread in swimming pools, saunas, gyms, or nail salons – places where you are likely to walk barefoot. Tight socks that hold in moisture may also be a contributing factor. Heat, humidity, and perspiration help spread the infection, which is highly contagious. A few natural remedies that may help reduce the fungus from spreading include applying tea tree, lavender, lemon, or thyme oils to the affected nails. A foot bath with baking soda or white vinegar may help too. However, if the nail condition persists or spreads it is suggested that you consult with a podiatrist for an examination and treatment plan.
If left untreated, toenail fungus may spread to other toenails, skin, or even fingernails. If you suspect you have toenail fungus it is important to seek treatment right away. For more information about treatment, contact one of our podiatrists of Palm Beach Foot & Ankle. Our doctors can provide the care you need to keep you pain-free and on your feet.
Symptoms
- Warped or oddly shaped nails
- Yellowish nails
- Loose/separated nail
- Buildup of bits and pieces of nail fragments under the nail
- Brittle, broken, thickened nail
Treatment
If self-care strategies and over-the-counter medications does not help your fungus, your podiatrist may give you a prescription drug instead. Even if you find relief from your toenail fungus symptoms, you may experience a repeat infection in the future.
Prevention
In order to prevent getting toenail fungus in the future, you should always make sure to wash your feet with soap and water. After washing, it is important to dry your feet thoroughly especially in between the toes. When trimming your toenails, be sure to trim straight across instead of in a rounded shape. It is crucial not to cover up discolored nails with nail polish because that will prevent your nail from being able to “breathe”.
In some cases, surgical procedure may be needed to remove the toenail fungus. Consult with your podiatrist about the best treatment options for your case of toenail fungus.
If you have any questions, please feel free to contact our offices located in Boynton Beach, Palm Beach Gardens, and West Palm Beach, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Toenail Fungus
Toenail fungus is a frustrating problem that affects many people. It can be persistent and hard to get rid of. As many different types of fungi are present throughout the environment, it is very easy to contract toenail fungus.
The feet are especially susceptible to toenail fungus because shoes and socks create the ideal dark and moist environment that fungal infections thrive in. While fungal infections of the nail plate are quite common, if left untreated they can spread beyond the toenail and into the skin and other parts of the body.
Signs of toenail fungus include a thickened nail that has become yellow or brown in color, a foul smell, and debris beneath the nail. The toe may become painful due to the pressure of a thicker nail or the buildup of debris.
Treatment for toenail fungus is most effective during the early stages of an infection. If there is an accumulation of debris beneath the nail plate, an ingrown nail or a more serious infection can occur. While each treatment varies between patients, your podiatrist may prescribe you oral medications, topical liquids and creams, or laser therapy. To determine the best treatment process for you, be sure to visit your podiatrist at the first signs of toenail fungus.
Causes and Caring for Blisters on the Foot
There are many causes of blisters, which are small sacs of fluid that form on the body. One of the main causes is new, tight, or ill-fitting shoes. The harder areas of the shoe can rub against your heels, soles, and toes, and if the friction is repeated for long periods, blisters often form. These become very painful, especially if you continue the activity. Excessive moisture or perspiration, which happens more frequently during warmer weather, may also cause blisters in runners. There are a few precautions you can implement to prevent blisters. Keep the feet dry and put powder on them to reduce sweating, as well as wearing moisture-wicking socks. Wearing softer, more flexible shoes can reduce the chance of a blisters formation and ceasing the activity will allow the skin time to heal on its own. If a blister pops open, is extremely large, or won’t heal, it is a good idea to seek the professional care of a podiatrist who can safely drain the area and help stave off infection.
Blisters are prone to making everyday activities extremely uncomfortable. If your feet are hurting, contact one of our podiatrists of Palm Beach Foot & Ankle. Our doctors can provide the care you need to keep you pain-free and on your feet.
Foot Blisters
Foot blisters develop as a result of constantly wearing tight or ill-fitting footwear. This happens due to the constant rubbing from the shoe, which can often lead to pain.
What Are Foot Blisters?
A foot blister is a small fluid-filled pocket that forms on the upper-most layer of the skin. Blisters are filled with clear fluid and can lead to blood drainage or pus if the area becomes infected.
How Do Blisters Form?
Blisters on the feet are often the result of constant friction of skin and material, usually by shoe rubbing. Walking in sandals, boots, or shoes that don’t fit properly for long periods of time can result in a blister. Having consistent foot moisture and humidity can easily lead to blister formation.
Prevention & Treatment
It is important to properly care for the affected area in order to prevent infection and ease the pain. Do not lance the blister and use a Band-Aid to provide pain relief. Also, be sure to keep your feet dry and wear proper fitting shoes. If you see blood or pus in a blister, seek assistance from a podiatrist.
If you have any questions, please feel free to contact our offices located in Boynton Beach, Palm Beach Gardens, and West Palm Beach, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Risk Factors and Treatment of Plantar Warts
Plantar warts are unsightly and can be painful. These small, hardened growths that form on the bottom of the foot are typically benign, but highly contagious. The Human Papilloma Virus (HPV), which is usually the primary cause, enters the body through a sore or crack in the skin. It generally affects the heels and the fleshy area at the base of the toes. The virus is found in moist places like communal pools, public showers, and gym locker rooms. It’s recommended to wear protective foot coverings in such areas to help prevent contact with the virus. It’s also important to avoid touching the warts, as the virus can be easily spread. Treatment options include over-the-counter medications, liquid nitrogen, which burns the callus off the foot, or cryotherapy which freezes the wart. If plantar warts are a recurring problem, it is strongly suggested to visit a podiatrist for a proper diagnosis and treatment plan.
Plantar warts can be very uncomfortable. If you need your feet checked, contact one of our podiatrists from Palm Beach Foot & Ankle. Our doctors will assist you with all of your foot and ankle needs.
About Plantar Warts
Plantar warts are the result of HPV, or human papillomavirus, getting into open wounds on the feet. They are mostly found on the heels or balls of the feet.
While plantar warts are generally harmless, those experiencing excessive pain or those suffering from diabetes or a compromised immune system require immediate medical care. Plantar warts are easily diagnosed, usually through scraping off a bit of rough skin or by getting a biopsy.
Symptoms
- Lesions on the bottom of your feet, usually rough and grainy
- Hard or thick callused spots
- Wart seeds, which are small clotted blood vessels that look like little black spots
- Pain, discomfort, or tenderness of your feet when walking or standing
Treatment
- Freezing
- Electric tool removal
- Laser Treatment
- Topical Creams (prescription only)
- Over-the-counter medications
To help prevent developing plantar warts, avoid walking barefoot over abrasive surfaces that can cause cuts or wounds for HPV to get into. Avoiding direct contact with other warts, as well as not picking or rubbing existing warts, can help prevent the further spread of plantar warts. However, if you think you have developed plantar warts, speak to your podiatrist. He or she can diagnose the warts on your feet and recommend the appropriate treatment options.
If you have any questions please feel free to contact our offices located in Boynton Beach, Palm Beach Gardens, and West Palm Beach, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
All About Plantar Warts
Plantar warts are warts that are only found on the feet, hence the term “plantar”, which means “relating to the foot.” They are caused by the human papillomavirus, or HPV, and occur when this virus gets into open wounds on the feet. The warts themselves are hard bumps on the foot. They are easily recognizable, mostly found on the heels or ball of the foot. Plantar warts are non-malignant, but they can cause some pain, discomfort, and are often unsightly. Removing them is a common step toward treating them.
Plantar warts can cause some pain while standing, sometimes felt as tenderness on the sole of your foot. Unless the wart has grown into the foot behind a callus, you will be able to see the fleshy wart. A podiatrist should only be consulted if there is an excessive amount of pain. Plantar warts are not cancerous or dangerous, but they can affect your walking and continually reappear. Anyone who suffers from diabetes or a compromised immune system disease should seek out care immediately.
Podiatrists are easily able to diagnose plantar warts. They usually scrape off a tiny bit of the rough skin to make tiny blood clots visible and examine the inside of warts. However, a biopsy can be done if the doctor is not able to diagnose them from simply looking at them. Although plantar warts usually do not require an excessive amount of treatment, there are ways to go about removing them. A common method is to freeze them off using liquid nitrogen, removing them using an electrical tool, or burning them off via laser treatment. For a less invasive treatment option, topical creams can be used through a doctor’s prescription. This treatment method takes more time, however. Keep the wart covered for protection in between daily treatments.
The best way to avoid developing plantar warts is to avoid walking barefoot in public places. Avoid this especially if you have open sores or cuts on your feet. It is also important to avoid direct contact with warts in general, as they are highly contagious.
How Often Should Orthotics Be Replaced?
Orthotics are inserts placed in your shoes to add cushioning that are often prescribed for people who have plantar fasciitis or other painful foot conditions. They can improve your gait and posture as well as help reduce pain. Orthotics can be made specifically to fit your foot, which increases their efficacy, and are either soft, semi-rigid, or rigid depending on the foot condition being treated. They last different durations based on materials, your weight, and the amount of activity you do. Replacement of orthotics can range from three-to-six months to several years. To help orthotics last longer wipe them with a damp – not wet – cloth, or use spray shoe cleaners. Wearing shoes that fit properly will also add to the lifespan of your orthotics. If you notice that your orthotics are fraying, smell bad, or are worn, they may be doing you more harm than good and probably need to be replaced. Please visit a podiatrist before deciding on which orthotics, inserts, or insoles are best for your feet. And check back with your podiatrist periodically to see if they need to be replaced.
If you are having discomfort in your feet and would like to try orthotics, contact one of our podiatrists from Palm Beach Foot & Ankle. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Are Orthotics?
Orthotics are inserts you can place into your shoes to help with a variety of foot problems such as flat feet or foot pain. Orthotics provide relief and comfort for minor foot and heel pain but can’t correct serious biomechanical problems in your feet.
Over-the-Counter Inserts
Orthotics come in a wide variety of over-the-counter inserts that are used to treat foot pain, heel pain, and minor problems. For example, arch supports can be inserted into your shoes to help correct overarched or flat feet, while gel insoles are often used because they provide comfort and relief from foot and heel pain by alleviating pressure.
Prescription Orthotics
If over-the-counter inserts don’t work for you or if you have a more severe foot concern, it is possible to have your podiatrist prescribe custom orthotics. These high-quality inserts are designed to treat problems such as abnormal motion, plantar fasciitis, and severe forms of heel pain. They can even be used to help patients suffering from diabetes by treating foot ulcers and painful calluses and are usually molded to your feet individually, which allows them to provide full support and comfort.
If you are experiencing minor to severe foot or heel pain, it’s recommended to speak with your podiatrist about the possibilities of using orthotics. A podiatrist can determine which type of orthotic is right for you and allow you to take the first steps towards being pain-free.
If you have any questions please contact our offices located in Boynton Beach, Palm Beach Gardens, and West Palm Beach, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
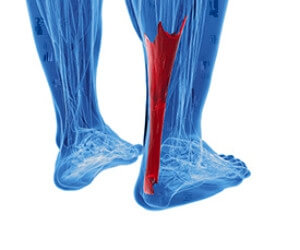
Causes of Achilles Tendonitis
 When the Achilles tendon, which is the large tendon on the back of the ankle connecting the calf to the heel bone, becomes inflamed, Achilles tendonitis occurs. Achilles tendonitis may not come from any particular trauma, but instead, the pain gradually worsens over time. Most of the time, pain from Achilles tendonitis is worse in the morning and after long periods of rest, and the pain lessens throughout the day. The most common cause of Achilles tendonitis is over-pronation which is when the arch of the foot flattens upon bearing weight and puts stress on the tendon. Other factors that can lead to Achilles tendonitis include poorly fitting shoes, poor stretching, trauma or a shortened tendon. Patients who are experiencing symptoms of Achilles tendonitis should consult a podiatrist, because it can eventually lead to a painful rupture of the tendon.
When the Achilles tendon, which is the large tendon on the back of the ankle connecting the calf to the heel bone, becomes inflamed, Achilles tendonitis occurs. Achilles tendonitis may not come from any particular trauma, but instead, the pain gradually worsens over time. Most of the time, pain from Achilles tendonitis is worse in the morning and after long periods of rest, and the pain lessens throughout the day. The most common cause of Achilles tendonitis is over-pronation which is when the arch of the foot flattens upon bearing weight and puts stress on the tendon. Other factors that can lead to Achilles tendonitis include poorly fitting shoes, poor stretching, trauma or a shortened tendon. Patients who are experiencing symptoms of Achilles tendonitis should consult a podiatrist, because it can eventually lead to a painful rupture of the tendon.
Achilles tendon injuries need immediate attention to avoid future complications. If you have any concerns, contact one of our podiatrists of Palm Beach Foot & Ankle. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is the Achilles Tendon?
The Achilles tendon is a tendon that connects the lower leg muscles and calf to the heel of the foot. It is the strongest tendon in the human body and is essential for making movement possible. Because this tendon is such an integral part of the body, any injuries to it can create immense difficulties and should immediately be presented to a doctor.
What Are the Symptoms of an Achilles Tendon Injury?
There are various types of injuries that can affect the Achilles tendon. The two most common injuries are Achilles tendinitis and ruptures of the tendon.
Achilles Tendinitis Symptoms
- Inflammation
- Dull to severe pain
- Increased blood flow to the tendon
- Thickening of the tendon
Rupture Symptoms
- Extreme pain and swelling in the foot
- Total immobility
Treatment and Prevention
Achilles tendon injuries are diagnosed by a thorough physical evaluation, which can include an MRI. Treatment involves rest, physical therapy, and in some cases, surgery. However, various preventative measures can be taken to avoid these injuries, such as:
- Thorough stretching of the tendon before and after exercise
- Strengthening exercises like calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses
If you have any questions please feel free to contact our offices located in Boynton Beach, Palm Beach Gardens, and West Palm Beach, FL . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.